Point-of-Care Ultrasound Diagnostic Tool Use on the Rise
Expand Skills and Bring Expertise to Your Practice With Point-of-Care Ultrasound
April 18, 2018
By Hillel Kuttler

A semi-conscious soldier was brought to a U.S. Army clinic in Tarin Kowt, Afghanistan, in 2005. He exhibited superficial wounds and no apparent head injuries from a training-exercise accident.
“It looked pretty benign, externally,” said Jonathan Monti, DSc, PA-C, RDMS, a captain on duty that day. “He was initially triaged as relatively minorly injured.”
A secondary survey, however, revealed blood gathered around the soldier’s heart. The patient was rushed to the operating room, where a pericardial window was performed, allowing the blood to drain. Shrapnel had penetrated the chest and then the heart. The shrapnel was removed and the patient saved.
The secondary survey had been done using a point-of-care ultrasound machine – the first time Monti used one. During downtime on his base, he’d read a booklet on operating the device.
“My outlook on point-of-care ultrasound changed at that point: Maybe you didn’t need to be trained as a radiologist to use ultrasound,” Monti, who retired from the military as a major and now works in Seattle for the Henry M. Jackson Foundation for the Advancement of Military Medicine, said of the 2005 episode.
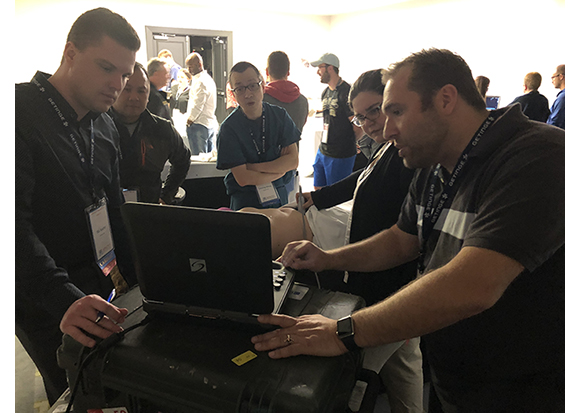
Today, PAs’ use of point-of-care ultrasound is growing. The Society of Point-of-Care Ultrasound, an AAPA special interest group founded by Monti and Frank Norman, a PA near Orlando, Florida, estimates 15 percent of PA programs have incorporated ultrasound instruction to some degree.
In 2015, Monti and Norman co-founded the Society of PAs in Clinical Ultrasound. The society received inquiries from physicians, nurse practitioners, medical students and others, leading the two in 2017 to broaden the group’s name to the Society of Point-of-Care Ultrasound (SPOCUS). SPOCUS now has 275 members and includes a Student Ultrasound Interest Section for those in PA programs lacking an ultrasound component.
SPOCUS’ goal is for all PA programs to have integrated ultrasound in their curricula by 2031.

Norman and Monti wrote guidelines for credentialing PAs in point-of-care ultrasound use. The 2017 guidelines state that “training in clinical ultrasound should begin at the earliest point of PA school to allow for the progression of skills through didactic and clinical training.” They go on to say that instruction “should begin with basic ultrasound physics and instrumentation, followed by a brief introduction to the clinical applications of bedside ultrasound.”
AAPA’s upcoming conference in New Orleans will include Yes I Scan, a question-and-answer competition involving students from 15 PA programs, and demonstrations on performing ultrasound scans, such as aortic ultrasounds. The session will help to highlight the advantages and multiple uses of point-of-care ultrasound, said one of its organizers, Miranda Ghali, who’ll be graduating in June from Nova Southeastern University PA Program’s Orlando campus.
Point-of-care ultrasound uses a small, portable machine – Monti compared its size to a laptop computer’s – with a cord leading to a transducer that, when placed near the patient’s skin, sends sound waves that bounce into the body and back, sonar-like, then converts them to digital images within seconds.
It allows users to examine the chest or abdomen for signs of bleeding due to trauma; perform a cardiac ultrasound to seek signs of fluid around the heart and a lung ultrasound for signs of pneumonia; and look at acute fractures and tendon tears.
It “can speed and guide your management of patients,” Monti said.
Rachel Krackov, a PA and an adjunct faculty member at Nova Southeastern, called it equipment that’s equivalent to an otoscope or a stethoscope.
The device is a significant timesaver in addressing very focused questions, rather than sending a patient for, say, a CT scan, Norman explained. “It makes for a better provider, and is much cheaper. An added benefit is that no radiation is involved,” he said.
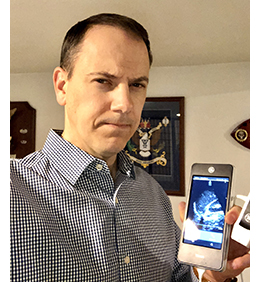
Cost and time constraints in PA programs are key factors that until now have worked against point-of-care ultrasound instruction. While standard ultrasound machines, normally associated with obstetrics, can cost $30,000, a point-of-care ultrasound can cost as little as $2,000. One model, which Krackov said could be a “game changer” for PA programs, is produced by Butterfly Network, connects to a smartphone, and includes three probes: for curvilinear, linear, and phased array examinations.
For a four-week, 16-hour course Krackov led for its PA students last summer, Nova Southeastern rented a dozen machines. The course included lectures, reading assignments, and practice time for scanning. All 62 students in the PA program participated in the voluntary course.
The program’s director, Lorilee Butler, PA-C, said she considered it important “to give students additional skills being used in clinics and hospitals.” Krackov had initially been a guest speaker in Butler’s class on medical imaging.
In the summer course, Krackov said she was energized by her students’ enthusiasm. “They’d say, ‘Oh, that’s the gall bladder!’ They could actually see what was going on with the organs. They’d say, ‘Come look at this,’ ” she remarked. “They’ve got the bug. It’s fun to teach them through a clinical scenario.”
Rachel Johnson, a Nova Southeastern student, had, with Ghali, proposed the summer course because she recognized its applicability in her career. Johnson would like to work in emergency medicine, where point-of-care ultrasound technology promises to be broadly available, but “if I get a job somewhere I don’t use ultrasound, it’ll be hard to get my certificate because I won’t have enough hours [on it],” she said.
Experience on the device will provide a deeper understanding of her patients’ anatomy and disease processes and help to “connect clinically with my patients and understand what they’re going through,” she said. “Career-wise, having this knowledge will open up more doors.”
Norman takes a similar view. “We think that PAs are the perfect professionals to be the directors of clinical ultrasound in their practices. A family practice or a dermatology clinic should have an ultrasound program. PAs are a natural fit to do that,” said Norman, who works in emergency medicine at the Heart of Florida Regional Medical Center.
“For example, you go to the doctor’s office due to abdominal pain. The doctor will send you out to get a CT scan to see if it’s a kidney stone. The ultrasound can quickly give the patient an answer and give the feedback to the provider on which way the treatment plan is progressing. There are so many barriers between us and the patient, but ultrasound is the first instrument I can think of that brings the provider back to the patient’s bedside.”
As training in point-of-care ultrasound is becoming more widespread in medical schools, PA programs can help their students keep pace, several interviewees stated.
“We are [physicians’] colleagues, so we should be able to do anything they want us to do. We can’t support them well if we don’t have the same basic skills,” said Krackov. “We’re using it to answer very specific questions: Is a gallstone there? Is a clot there? Is there a bowel obstruction?”
Krackov, who founded a Tampa-area company, Practical Point of Care Ultrasound Consultants, became interested in the device’s potential while working in interventional radiology. A radiologist she worked with suggested that Krackov get credentialed in ultrasound use, and she did – as a registered vascular specialist.
A “hot issue” now, she said, is whether those using a point-of-care ultrasound should need to be credentialed. Krackov believes that the credentialing helped her. “I feel that PAs should have the option of getting a point-of-care ultrasound credential if they want it,” she said. “It’s all about the options, so you can serve your patients best.”
One patient encounter in 2007, at Rhode Island’s Roger Williams Medical Center, dramatized for Krackov the device’s utility.
The patient came in distressed and short of breath. An x-ray revealed a whitened lung – possibly pneumonia. Using a point-of-care ultrasound, Krackov saw a large effusion that had collapsed the patient’s lung. Krackov then performed a thoracentesis and used the ultrasound to position a needle to drain the fluid.
“It was very safe. It would’ve been very dangerous if you did it without ultrasound guidance. We were able to stabilize her, expand her lungs – all with an ultrasound,” she said. “I thought: Why don’t we use it to look at everything?”
As to Monti: He went on to do doctoral research on the ultrasound, and taught medics and even food-service inspectors to use the device. A lesson covering the very basics took as little as 10 minutes.
His current work at the Jackson Foundation involves evaluating the training required to prepare PAs, military medics, and nurses to use point-of-care ultrasound.
While point-of-care ultrasound machines have become smaller and thus more portable, the images much clearer and the cost far cheaper, “the greatest barrier [today] is the availability of training opportunities,” Monti said. “We still haven’t adequately addressed how to [widely] employ and use the machines.”
Hillel Kuttler is a freelance writer. Contact him at [email protected].
Thank you for reading AAPA’s News Central
You have 2 articles left this month. Create a free account to read more stories, or become a member for more access to exclusive benefits! Already have an account? Log in.



