PA Diagnosed with Ebola Suffers Trauma After Long Isolation
Preston Gorman Recovered but Felt the Effects of It for Years Afterward
April 1, 2020
By Jennifer Walker
In March 2015, Preston Gorman, PA-C, was isolated in a room at a medical facility in Kailahun, West Africa. He had been diagnosed with the Ebola virus and was waiting to be transported to the National Institutes of Health (NIH) in Bethesda, Maryland, for treatment. While he waited, Gorman, a PA in urgent care at the University of Texas in Austin, repeatedly had three thoughts: He dreaded the symptoms he knew would come with Ebola, which could include seizures and delirium; he wanted to hang on long enough to make it home; and he prayed to God that once he was home, he would survive.
After arriving at NIH, Gorman was on a ventilator for 10 days and isolated for nearly a month. He recovered from Ebola, but he struggled with feelings of loneliness and disconnection for years afterward. This hit home two weeks after leaving NIH and returning to Texas, when his parents threw him a party at their house. “At that party, where people are celebrating and everyone is so happy, I was thinking, ‘I’m supposed to be happy. Why am I not happy?’” he says. “I was deeply confused.”
Gorman later recognized that he was going through trauma, in part because of the amount of time he spent in isolation. Today, thousands of people in the United States who have already been diagnosed with coronavirus have been and will be cut off from social contact for extended periods of time. That number jumps to more than 750,000 people worldwide as of March 31, 2020. While not exactly the same, people affected by coronavirus are experiencing a lack of social contact that has similarities to Gorman’s story.
“You can’t really change the way [patients] are treated,” Gorman says about isolation and quarantine practices for viruses like Ebola and coronavirus. “But we should be aware that this type of experience can have a deep psychological impact on a person.”
Volunteering in Africa
After five years as a firefighter and a paramedic, Gorman wanted to have a bigger role in medicine. He attended the PA program at Baylor College of Medicine in Houston, Texas, graduated in 2012; and worked in family medicine at a private clinic in Baytown, Texas. Then in 2015—in the middle of the biggest Ebola epidemic in West Africa—Gorman decided he wanted to volunteer there. “I just felt a calling to go,” he says.
After training for a week in Freetown, the capital of Sierra Leone in West Africa, Gorman, who was a volunteer with Partners for Health, went to the Ebola Treatment Unit (ETU) in Maforki. Patients who arrived at the ETU had to have three of the seven symptoms that indicate Ebola—these include high fever, chills, vomiting, abdominal pain, diarrhea, headaches, and hiccups—to be admitted to the unit for testing and treatment. Gorman spent three days at the unit.
He was then transferred to a government hospital in Port Loko, where he worked in the men’s ward. Patients were treated for malaria, tuberculosis, and wounds. Those who were suspected of having Ebola were turned away at the door with instructions to go to the ETU.
After one and a half weeks at the hospital, Gorman passed out during a morning meeting. It was hot outside and the hospital lacked air conditioning, so everyone, including him, thought he was dehydrated. He went back to the volunteer camp in Maforki to rest, then woke up the next morning with a 102.9 fever.
“From that point forward, I was isolated,” he says.
Ebola Diagnosis and Treatment

At the camp, Gorman’s belongings – with the exception of a flip phone – were burned. Gorman was told to put on a Tyvek suit and to take an ambulance to the British facility for healthcare workers in Kailahun, two hours away. After getting in the vehicle, “I promptly vomited all over the back of the ambulance,” he says. He rode alone in the back for the duration of the trip.
At the British facility, Gorman was diagnosed with Ebola. He remembers being treated with IV fluids and taking Zofran for nausea. He continued to vomit and started having diarrhea. He made two phone calls: one to his mom and one to his dad to tell them about his diagnosis. And he waited while staff arranged a flight for him to the United States.
Two days later, Gorman traveled for four hours to the airfield, then boarded a plane with an infectious disease unit in the back for the long flight. “That was probably the most miserable 16 hours of my life,” he says. “I continued to have symptoms all throughout the flight. I also had a lot of pain. My whole body hurt, kind of like the flu, but way worse. I didn’t have a watch so I couldn’t keep track of time. I couldn’t tell how long it had been or how much longer it would be. It was horrific.”
When he arrived at Dulles International Airport in Virginia, Gorman was put in a long plastic bubble then transported to an ambulance, where he rode with one physician and one nurse to NIH. This was the first time since his diagnosis that he didn’t have to travel alone. At NIH, Gorman was taken to an isolation unit, where the bubble was removed, and he began treatment.
During the next 12 days, which included 10 days of intubation, Gorman’s immune system began to fight the virus. On the 12th day, the tube was removed from his mouth and he was disconnected from the ventilator. He immediately tried to stand up with the help of two providers and lasted for 10 seconds before he collapsed in exhaustion. It would be an arduous road to recovery.
Gorman continued to test positive for Ebola for the next one to two weeks, which is why he was in isolation for nearly a month. For the first two days after he was taken off the ventilator, he could only have water twice a day by sucking on a small, wet sponge attached to a stick. But then he could eat and drink again, which helped pass the time. He also talked on the phone to his family and friends, watched March Madness basketball on TV, and slept a lot.
When Gorman came out of isolation, the first person he saw was his mom, and he gave her a giant hug. “It felt really great to have human contact again for the first time in a month,” he says.
But Gorman also felt confused and overwhelmed around loved ones who hadn’t been through the same experience. “For them the story was over,” he says. “And for me, I was just waking up. I went into the ICU as one person and I came out another person. They were greeting the old Preston, but I was going to have to figure out who the new version of me was.”
Identifying Trauma
For the next year and a half, Gorman continued to live in a foggy, confused state. He felt disconnected from his body and the people around him, and he didn’t understand why. “I put on an external face as best I could, but I was lost all the time,” he says. “Everyone just expected me to move on without any help. No one really seemed to care.”
After living with his parents for the first year, Gorman’s relationship with them deteriorated, and they don’t speak today. He broke up with his girlfriend at the time. And he lost most of his friendships (though he is trying to repair some of those relationships today).

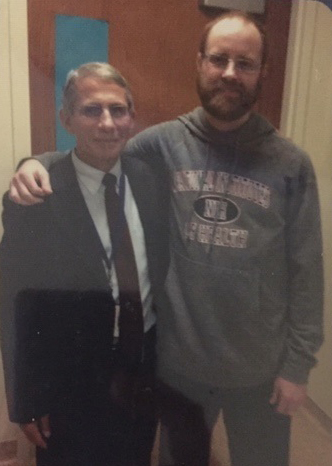
Then, in the fall of 2016, Gorman started seeing a therapist who identified what he was going through as trauma. He continued to see the same therapist for two years, which helped, as did his relationship with God. He read stories about Vietnam veterans, who he could identify with because the experience of coming back from Ebola felt a little like the experience of coming back from war. Gorman also read a lot of books about trauma, including The Body Keeps the Score. In 2017, he took copies of this book to the providers at NIH, where he was treated.
Asked why he passed out the books, Gorman says, “Physical symptoms can come from emotional trauma, [and as a provider] if you just see the symptoms and you don’t look behind them, then you completely miss what’s causing the problem for the patient. You instead cover it up with medication and they never actually heal. And this book explains that so well.”
Today, Gorman is aware of the effects of unprocessed trauma when he is treating his patients. Sometimes, if they are crying, anxious, panicked, or depressed, Gorman will acknowledge that part of their experience and tell them that their tears and other feelings and reactions are welcome. “You have to hold emotional space for the patient,” he says. “I want other PAs to know that sometimes what patients need more than anything else is to have that wounded place within them respected and honored.”
Read More
Rush University PAs Integral to Coronavirus Response
Africa Calls PAs: Providing Medical Care on the Continent
Providing Medical Care in Liberia Inspires Chicago PA to Continue Global Healthcare Commitment
An Ebola Patient Treated in the U.S. Chose to Remain Anonymous. Now He’s Telling His Story.
Jennifer Walker is a freelance writer in Baltimore, MD. Contact Jennifer at [email protected].
Thank you for reading AAPA’s News Central
You have 2 articles left this month. Create a free account to read more stories, or become a member for more access to exclusive benefits! Already have an account? Log in.



